Realising the potential of autotaxin inhibition in cancer
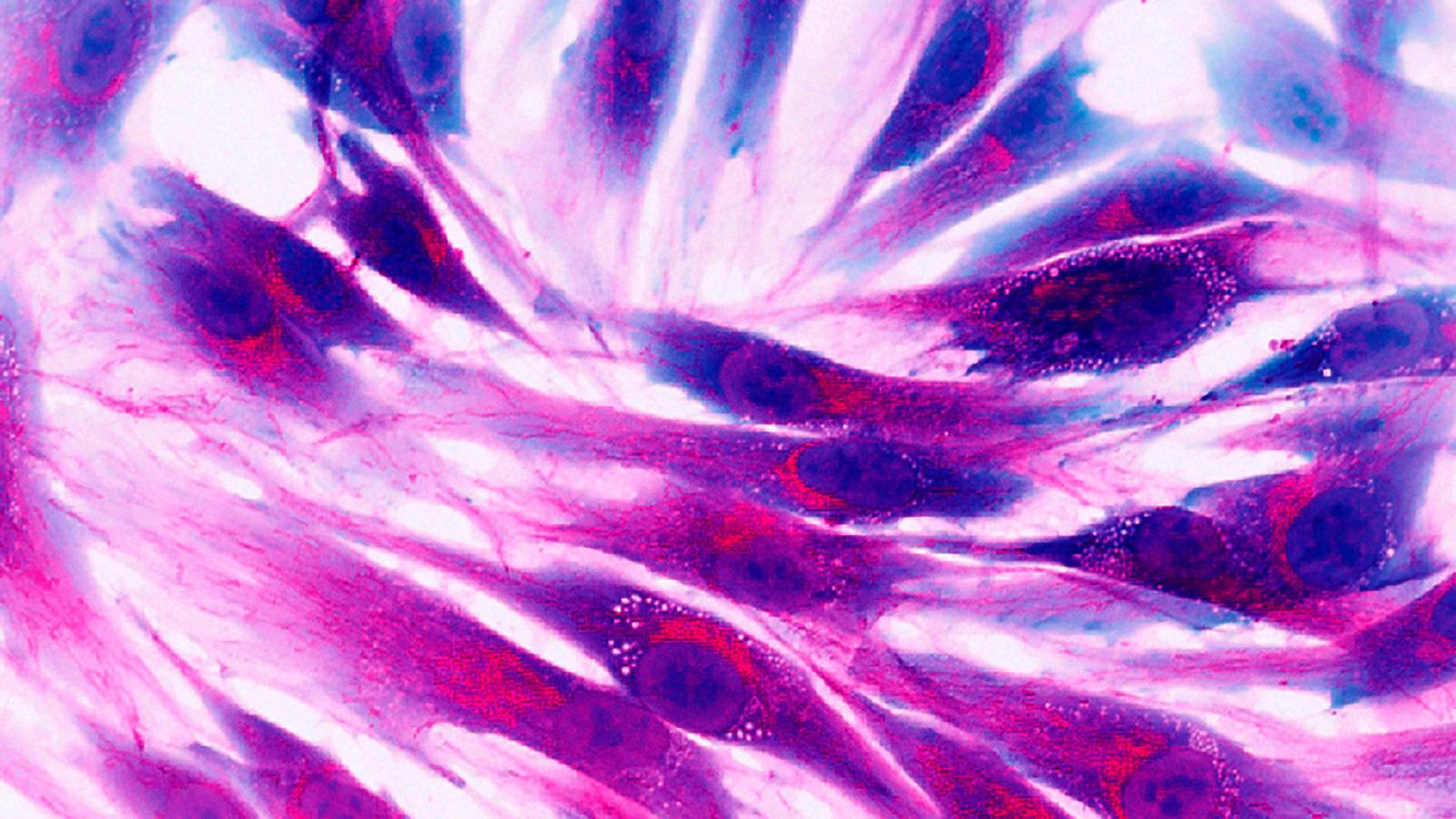
Tackling the fibroblast cells that form scar tissue around tumours takes down a barrier that prevents or inhibits the effect of many therapies.
There’s an increasing focus on using drugs to modify the tumour microenvironment, breaking down this blockade that supports tumour development and preventing penetration of cancer-killing immune cells. Scientists are looking at a range of different drug classes, such as lysyl oxidase (LOX) inhibitors and NADPH-oxidase inhibitors – but an obvious choice is a class of drugs known as autotaxin (ATX) inhibitors.
ATX inhibitors and fibrotic diseases
ATX inhibitors work by preventing the action of the enzyme, first discovered in the early nineties, which converts the precursor lysophosphatidylcholine (LPC) into a signalling molecule known as lysophosphatidic acid (LPA). These signals can induce various responses along multiple cellular signalling pathways that lead to a build up of fibroblasts.
Currently, there are no approved ATX inhibitors, but they are being studied in fibrotic diseases; although, in 2021, one of the leaders in the field, Gilead, suffered a setback when its ziritaxestat failed in the phase III ISABELA study in the lung scarring disease idiopathic pulmonary fibrosis (IPF).
But other companies continue to see the potential of this drug class in cancer and fibrotic diseases. One such is iOnctura, a biotech based in Amsterdam and Geneva, which points out that ATX also directly promotes cancer cell division and prevents the host making an immune response against the cancer. Thus, targeting this pathway may promote synergistic anti-cancer effects.
With supportive preclinical and early-stage study data recently published in the peer-reviewed journal Immuno-Oncology and Technology (IOTECH), iOnctura is eyeing the next stage of development with its ATX inhibitor, IOA-289, initially in combination with standard-of-care chemotherapy in pancreatic cancer.
Giusy Di Conza, head of research at iOnctura, said: “We chose pancreatic cancer because it is highly fibrotic. The fibrosis is immunosuppressive and impairs access to chemotherapies, which makes this disease very difficult to treat.”
Hilary Sandig, group leader at Cancer Research Horizons, an innovation unit that is part of Cancer Research UK, added that ATX inhibitors also disrupt intercellular signals within the tumour, adding another anti-tumour effect. “It is very encouraging to see that inhibiting ATX can impair this crosstalk and lead to antitumoural effect,” Sandig said.
Learnings from historic combination trials and avoiding toxicity
According to Di Conza, the presence of ATX is a “stress signal”, indicating hypoxic conditions surrounding the tumour and the presence of a feedback reaction, whereby cancer cell proliferation is boosted while immune responses from tumour targeting T-cells are suppressed.
But there are challenges to be overcome as the early generations of ATX inhibitors resulted in substantial toxicity. This became most apparent with Galapagos and Gilead’s ziritaxestat, which was trialled in combination with pirfenidone and nintedanib in IPF. Numerically higher mortality rates in the treatment arm, combined with a lack of efficacy meant that Gilead and Galapagos opted to end development of ziritaxestat. It’s still not clear what caused the toxicity issues in the negative readout from the phase 3 ISABELA studies announced in 2021. But Di Conza said that iOnctura’s data from IOA-289 is encouraging on the safety front, noting that another competitor in the ATX field, Blade Therapeutics, ran a study suggesting that interaction between the drugs in the combination could have led to the toxicity seen in ISABELA.
Di Conza also noted that they hadn’t seen any toxicity in “a healthy volunteer study”.
These findings have given iOnctura confidence for an ongoing AION-02 study with standard chemotherapy in metastatic pancreatic cancer patients.
There is also the potential for the drug to be used in other cancer indications, such as breast cancer, following supportive preclinical data published earlier this year. Combining the drug with immunotherapy is another logical step, given that scar tissue surrounding tumours has been blamed for several clinical trial failures in this branch of cancer research. The theory is that the wall of cells surrounding the tumour hinders or inhibits the influx of T-cells following the action of checkpoint inhibitor drugs.
Investigations in NASH and inflammatory diseases
Experts and KOLs discussed IOA-289 at an iOnctura ATX Symposium, held in Naples, Italy in May 2023. And Gianluigi Giannelli, scientific director of the National Institute of Gastroenterology "Saverio de Bellis", Research Hospital, Bari, Italy, said that there is potential, also, in stomach cancer, based on preclinical data. He told the symposium: “We are testing IOA-289 in several types of GI tract cancer. It is rare to see that a small molecule has both antiproliferative and antimigratory effect in all the cell lines tested.”
Further lines of investigation for ATX inhibitors include non-alcoholic steatohepatitis (NASH), the fatty liver disease that shows rising global incidence and puts patients at high risk of developing liver cancer.
ATX is also linked to inflammation-related diseases such as ulcerative colitis, and systemic sclerosis, where scar tissue builds up in internal organs, a potentially life-threatening condition (See BOX).
BOX: Autotaxin inhibitors in development
| Company | Drug | Indication | Stage |
|---|---|---|---|
| Mitsubishi Tanabe Pharma | MT-5562 | Systemic sclerosis | Preclinical |
| Bridge Biotherapeutics | BBT-877 | IPF | Phase 2 |
| Blade Therapeutics | BLD-0409 (cudetaxestat) | IPF | Phase 2 |
| iOnctura | IOA-289 | Pancreatic cancer/solid tumours | Phase 1b/2 |













