WHO clears Oxford malaria jab for immunisation programmes
The World Health Organization (WHO) has recommended the use of a malaria vaccine developed at Oxford University in the UK, after concluding it is 75% effective at protecting children from infection.
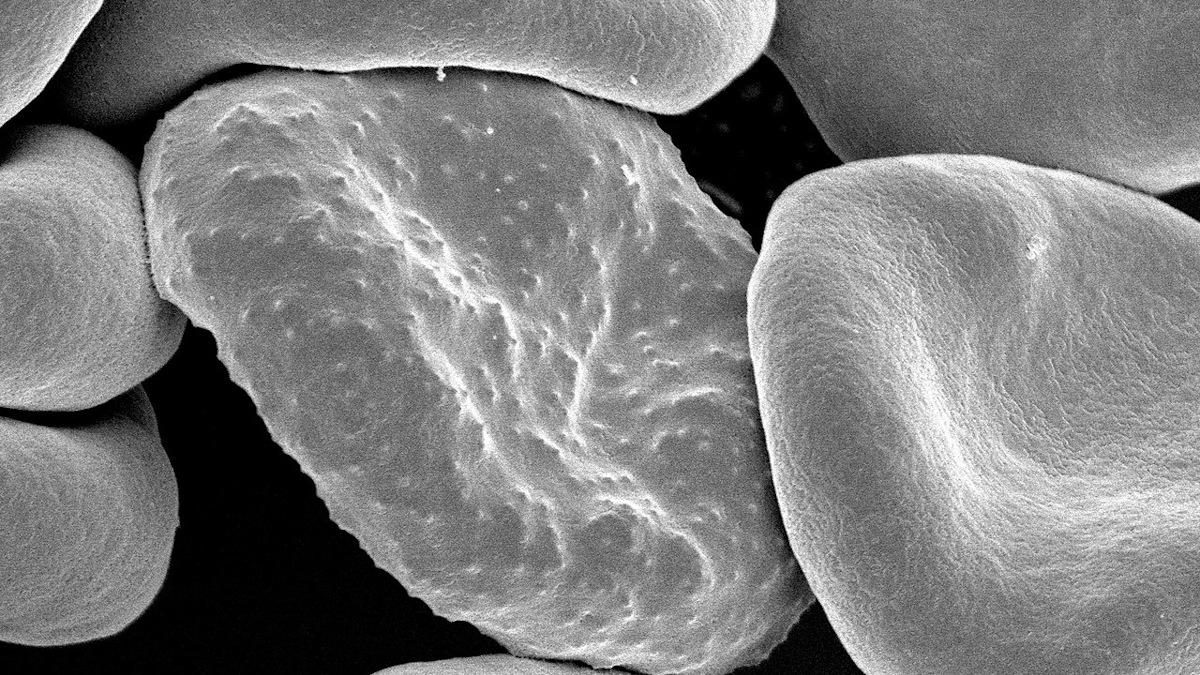
The pre-qualification of the shot by the WHO’s Strategic Advisory Group of Experts (SAGE) and the Malaria Policy Advisory Group (MPAG) means that the R21/Matrix-M vaccine is considered to have met the necessary standards of quality, safety, and efficacy to allow it to be used by national health systems.
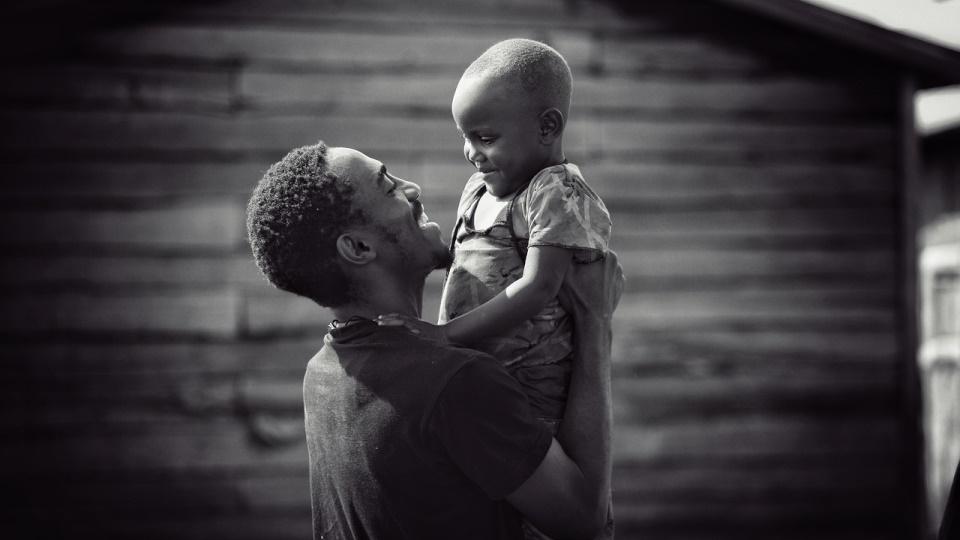
The most recent data from the WHO shows that there were 619,000 deaths from malaria worldwide in 2021, out of 247 million cases. All told, 95% of all cases are in Africa, and children under five are the most vulnerable to the parasite, accounting for 80% of all deaths in Africa.
The Oxford vaccine is given in four doses and, according to a clinical trial, was 75% effective at preventing malaria over 12 months in a trial involving 4,800 children in West Africa. Follow-up data from the study reported a year ago showed that the efficacy was maintained at 70% to 80% over two years.
In another recent development, India’s Serum Institute – the biggest vaccine manufacturer in the world and a major supplier of the AstraZeneca COVID-19 vaccine during the pandemic – has agreed to produce 100 million doses of the vaccine each year at a cost of $2 to $4 per dose.
The vaccine is the second to be given a green light by the WHO after GSK’s Mosquirix (RTS,S), which was pre-qualified by the WHO two years ago. That has shown protective efficacy of around 39% in its clinical trials - still sufficient to be used in some high-risk areas - and costs roughly twice as much as the Oxford jab.
Since 2019, only around 1.7 million doses of RTS,S have been distributed, as supplies have been limited. The approval of R21 – coupled with its ease of manufacture and modest cost – means that large-scale malaria immunisation programmes will be possible for the first time.
“As a malaria researcher, I used to dream of the day we would have a safe and effective vaccine against malaria. Now, we have two,” said Dr Tedros Adhanom Ghebreyesus, WHO Director-General. “Demand for the RTS,S vaccine far exceeds supply, so this second vaccine is a vital additional tool to protect more children faster, and to bring us closer to our vision of a malaria-free future.”
At least 28 countries in Africa plan to introduce a WHO-recommended malaria vaccine as part of their national immunisation programmes.
R21 uses an adjuvant developed by Novavax to boost the immune response. The company’s chief executive, John Jacobs, said that the new designation “highlights the meaningful contribution that R21/Matrix-M is likely to have in accelerating and expanding access to a safe, efficacious, and potentially life-saving vaccine to control malaria.”
WHO also issued recommendations on the advice of SAGE for new vaccines for dengue and meningitis, along with immunisation schedules and product recommendations for COVID-19.
Image by Siloé Amazzi from Pixabay.