UK digital health project aims to tackle dysfunctional breathing
A collaboration between academic centres in the UK has won government funding for a digital approach to dysfunctional breathing or dyspnoea, a symptom that affects around 10% of the population.
The Engineering and Physical Sciences Research Council (EPSRC) has set aside £400,000 (almost $490,000) for the project, which will help fund work at the Universities of Plymouth, Salford and Stirling, and the Glasgow School of Art.
The money will go towards a project – called OptiMuscle – that aims to develop a 'biofeedback' system that will allow people to see and hear how their muscles are working as they inhale and exhale – and help them to learn how to breathe better.
It would provide an alternative to standard breathing exercises for patients with conditions that affect breathing, including long-term respiratory diseases like asthma, chronic obstructive pulmonary disorder (COPD) and cystic fibrosis, which can be resource-intensive as they require patients to be overseen by a healthcare worker. Correcting dyspnoea can lead to improvements in breathlessness, hyperventilation and dizziness.
"This new system could revolutionise the way in which we manage breathing disorders. It will give people a window into their body, allowing them to see in real-time how their breathing muscles work," said Dr Steve Preece, research centre director at Salford, who is leading the project.
"In the future, we hope to expand this approach so it could be used to treat other health conditions which are related to altered muscle functioning."
That could include musculoskeletal pain, mobility in older people, anxiety-related disorders and long COVID, according to the researchers.
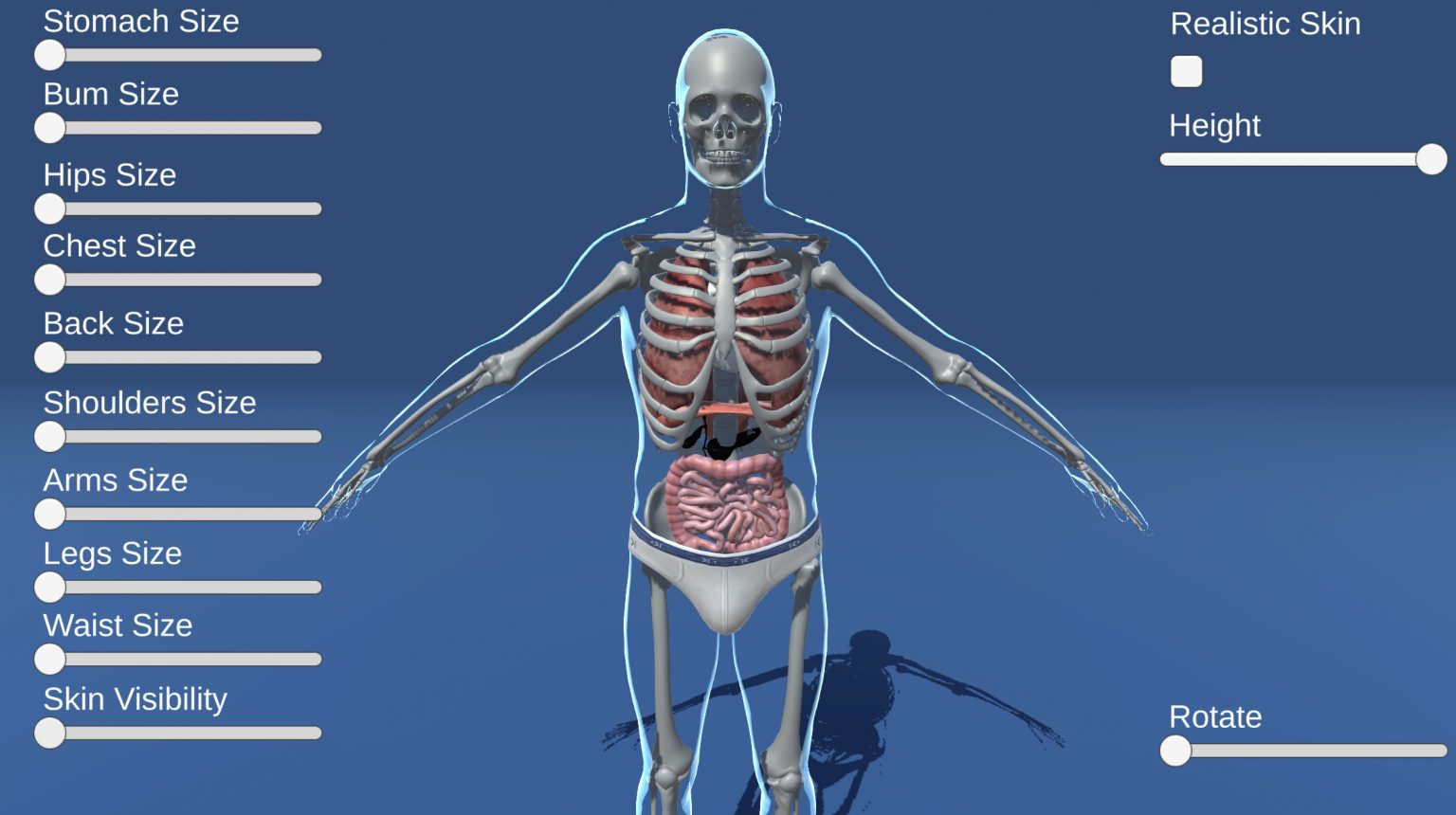
The first stage of the project will work to develop software that can produce an 'avatar' matched to the body shape of the user, which will be able to display geometrical changes in body shape during breathing, according to the partners. Using 3D cameras and body sensors, patients will be able to see and hear their breathing on screen.
It is anticipated that patients will initially use the digital tool in collaboration with a physiotherapist, re-educating their muscles for effective breathing.
Ultimately, however, the plan is to develop a fully autonomous system that patients can use at home to reduce the time they are in clinics. That would contribute towards the NHS Long Term Plan to provide digitally-enabled care across the UK, according to the team.
"Currently, in the UK, clinical assessments and treatments for dysfunctional breathing rely on visual assessments and breath-holding tests/questionnaires without validated tools to measure muscle patterns," said Professor Eduardo Miranda, who heads the Interdisciplinary Centre for Computer Music Research at Plymouth.
"By tapping into the visual and audio potential of digital technology, we can empower patients to change unhealthy behaviours and improve their breathing – while freeing up clinicians at the same time," he added.













