Oral ketamine set for pivotal trials in resistant depression
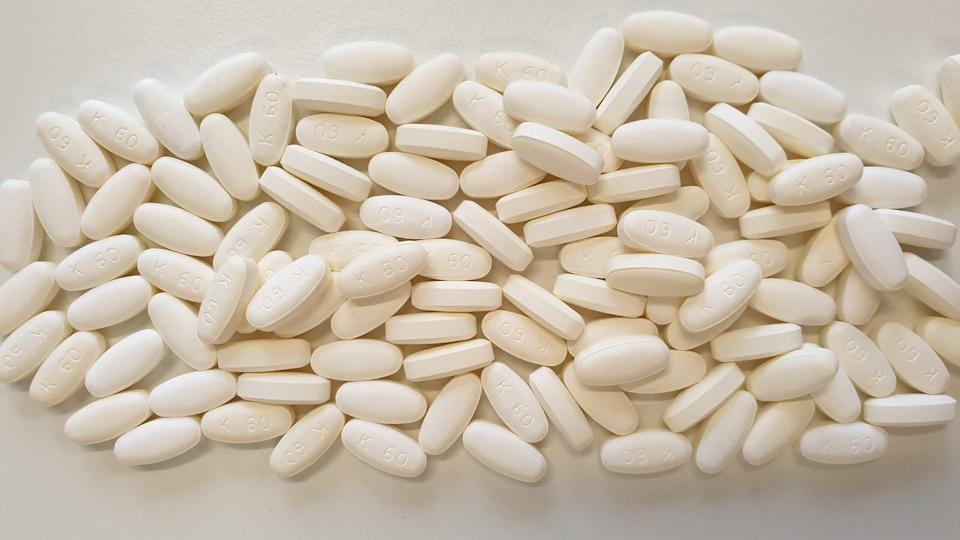
R107 extended-release ketamine tablets, Douglas Pharmaceuticals
A mid-stage trial of oral ketamine tablets has shown promising results in treatment-resistant depression (TRD), setting up a phase 3 programme and a possible challenge to Johnson & Johnson’s Spravato.
New Zealand-based contract manufacturing organisation Douglas Pharmaceuticals – which sponsored the 329-patient BEDROC trial and supplied the ketamine tablets – is now planning a phase 3 programme that could support regulatory filings.
The results have been published in the journal Nature Medicine and showed that a 180 mg dose of extended-release ketamine (R-107) was able to achieve a statistically significant improvement in symptoms compared to a placebo, measured using the Montgomery–Asberg Depression Rating Scale (MADRS). Other dosages were not significantly more effective than control.
It’s a significant finding because, to date, most studies of ketamine in depression have relied on either intravenous or intranasal administration, the latter resulting in the approval of J&J’s Spravato (esketamine) for TRD in 2019 and for major depressive disorder (MDD) with acute suicidal ideation or behaviour a year later.
Globally, the take-up of Spravato was modest in the post-launch period, but has started to gather momentum of late, with sales last year rising 80% to $689 million. Another 72% increase to $225 million in the first quarter of the year puts the drug on course to achieve sales above the blockbuster threshold of $1 billion for calendar 2024.
The new study involved daily dosing with oral ketamine for five days to identify patients seeing a benefit with the drug, which was followed by 12 weeks of twice-weekly dosing at 30, 60, 120, and 180 mg, or placebo, among responders.
There was a 6.1-point difference between ketamine 180 mg and the placebo group on MADRS by the end of that period, which was statistically significant and indicates a “clinically meaningful” change, according to the investigators, led by Paul Glue of the University of Otago in Dunedin, NZ.
The study also showed a dose-response relationship on secondary endpoints like remission and relapse rates. Side effects seen with IV and intranasal ketamine like dissociation, sedation, and increased blood pressure were also minimal, with the most common adverse reactions including dizziness and headache.
Overall, the researchers say the study demonstrated the feasibility of oral ketamine as a TRD treatment, pointing out that this can be carried out largely without clinic visits. They also note that the oral tablets would be less prone to abuse and diversion than other ketamine formulations. They could also be cheaper, given that Spravato's US list price in the US is $590 to $885 for two doses.
“Use of an extended-release oral dosage ketamine formulation may be advantageous compared with intranasal or intravenous dosing, in terms of reduced intensity of dissociation, lower risk of abuse, reduced frequency and intensity of sedative and cardiovascular side effects, and improved convenience for administration in the community,” they conclude.
According to Dr Paul Keedwell, consultant psychiatrist and fellow of the Royal College of Psychiatrists (RCP) in the UK, the study affirms the “impressive” antidepressant effect of ketamine, but in a more convenient and more tolerable form.
“Over 70% of depression sufferers who had failed to improve with an average of over four different antidepressants responded to oral ketamine and over 50% went into complete remission,” he said.
“Their results suggest that many will continue to do well with longer-term treatment, provided higher doses are used, but more research is needed with higher numbers of patients.”
Another company developing an oral ketamine candidate for TRD is Ketabon – a joint venture between HMNC Brain Health and Develco Pharma – whose KET01 formulation has shown improvements in depression symptoms in early-stage clinical studies, with low rates of dissociation or cardiovascular effects.













