NICE backs use of post-stroke genetic testing
NICE has launched a new consultation on the use of CYP2C19 genotype testing to guide treatment after a stroke or transient ischaemic attack (TIA) or ‘mini-stroke’.
CYP2C19 testing is carried out to see if patients will have resistance to treatment with clopidogrel, an anti-platelet therapy that is recommended by NICE as a treatment option for people at risk of a secondary stroke.
According to the health technology assessment (HTA) agency, some people with variations in the CYP2C19 gene could see a greater benefit with alternative drugs because they do not metabolise clopidogrel fully. Evidence has suggested that people with these variants have an increased risk of another stroke when taking clopidogrel compared to those without them.
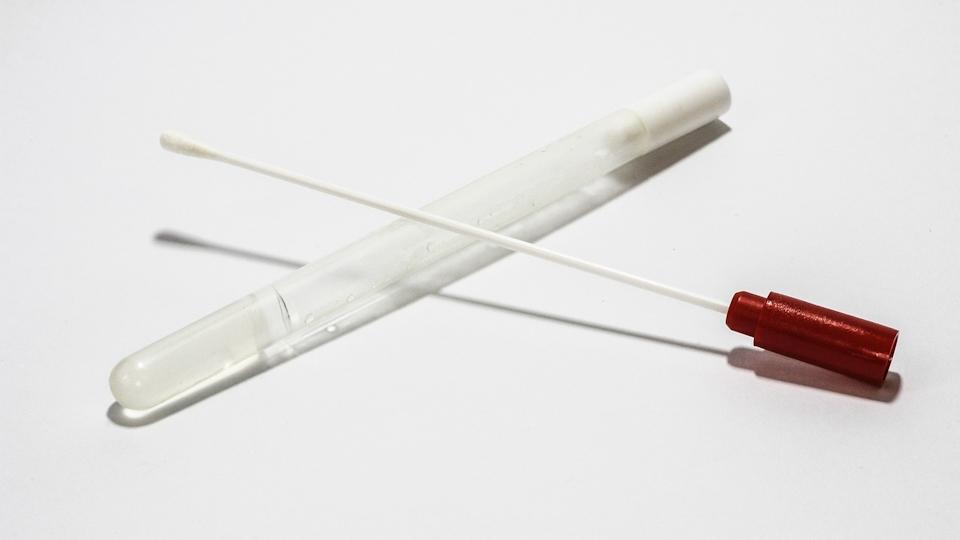
Last year, UK molecular diagnostics company Genedrive was awarded UKCA marking registration for its point-of-care (POC) CYP2C19-ID test, clearing the way for commercialisation in the UK, and before that got preliminary backing from NICE for its use in draft guidance, concluding that it was likely to save costs and increase life expectancy compared with no testing.
The latest draft says laboratory-based CYP2C19 genotype testing is the preferred first-line approach to testing, followed by Genedrive’s point-of-care kit, with another POC test from Genomadix an option if those are not available. NICE’s consultation on it will last through 26th April, with a final recommendation expected on or around 10th July.
Genedrive said in a statement that it will pursue the commercialisation of its test in the UK after that final NICE decision, and that it is also in the process of getting CE mark approval in the EU.
In comments on the initial draft guidance, the British and Irish Association of Stroke Physicians (BIASP) pointed out that only around 600,000 genotype tests are carried out in England alone per annum, and there would need to be an increase in capacity of more than 15% just to complete the genotype testing for clopidogrel resistance alone.
“We recognise that capacity within laboratories will need to increase before everyone who has had a new stroke or ‘mini-stroke’ can receive testing,” said Prof Jonathan Benger, NICE’s chief medical officer.
“While point-of-care testing is an alternative, our committee has identified that initially those people who could benefit most from laboratory-based testing are those who have had a non-minor stroke,” he added.
Around 35,850 people in England, Wales, and Northern Ireland have a non-minor stroke each year, according to NICE, and it is estimated that around a third of people in the UK have CYP2C19 gene variants. Meanwhile, around 11 million items of clopidogrel are dispensed each year at a cost of around £16 million to the NHS.
The prospect of a genetic test that could offer personalised care for patients having a stroke or TIA has been welcomed by the Stroke Association, which said: “We know that many stroke survivors spend the rest of their lives fearing another stroke, so it’s great to see that more people could be given appropriate help to significantly cut their risk of recurrent stroke.”