BMS’ LAG-3 RELATIVITY theory fails futility test

Bristol-Myers Squibb has abandoned a bid to extend the indications of its combination of PD-1 inhibitor Opdivo and LAG-3 inhibitor relatlimab into colorectal cancer after it failed the phase 3 RELATIVITY-123 trial.
The trial of the fixed-dose combination of the two drugs – already approved as Opdualag (nivolumab and relatlimab) for skin cancer melanoma – has been abandoned after an interim analysis suggested it would be unlikely to show a positive result.
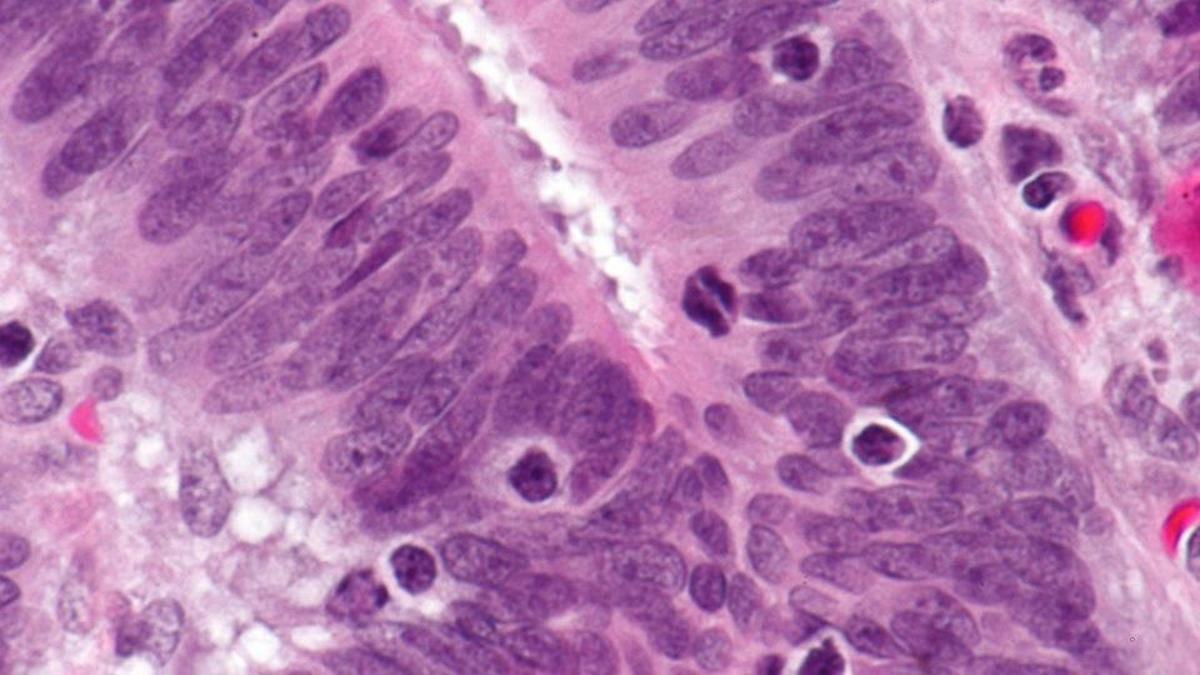
RELATIVITY-123 recruited 700 patients with microsatellite stable (MSS) metastatic colorectal cancer (mCRC) whose disease has progressed following at least one, but no more than four, prior lines of therapy.
The trial’s independent data monitoring committee has said the combination was likely to miss the primary endpoint of the trial, but there was no indication of any safety issues with the regimen.
The result is disappointing for BMS, which was first to market with a drug in the LAG-3 inhibitor class ahead of rivals like MSD with favezelimab, also in late-stage testing for PD-L1-positive mCRC as a fixed-dose combination with PD-1 inhibitor Keytruda (pembrolizumab). Results from that study are due next year.
Other LAG-3 drugs in the pipeline include Immutep’s soluble LAG-3 protein eftilagimod alpha, Novartis/Immutep’s leramilimab, Incyte’s retifanlimab and Regeneron’s fianlimab, in mid-stage trials for various forms of cancer.
BMS said the nivolumab/relatlimab combination remains in development for other cancer types, including hepatocellular carcinoma (HCC) and non-small cell lung cancer (NSCLC), but that the results in mCRC are very disappointing. Opdualag has been growing well since it was first approved in 2022, bringing in $430 million in the first nine months of 2023, up from $148 million in the same period of 2022.
“Metastatic colorectal cancer is a challenging cancer to treat with high unmet needs,” said Jeffrey Walch, BMS’ global programme lead.
“Though there have been advances in treating patients with microsatellite instability-high (MSI-H)/deficient mismatch repair (dMMR) colorectal cancers, patients with microsatellite stable (MSS) tumours continue to have limited treatment options in later lines of therapy,” he added.
Like PD-1, LAG-3 is a negative regulator of T-cells, suppressing their activity against cancer cells, so, when that brake is released, the immune system can attack and kill tumours.
Walch noted that immunotherapies have typically been unable to show much efficacy in MSS tumours, but BMS had “hoped to demonstrate meaningful clinical benefit in this patient population.”
RELATIVITY-123 explicitly excluded patients with MSI-H and dMMR tumours. The study will be followed up to explore the effects of the combination in this mCRC setting more fully.