Around 3.4m people infected with coronavirus in England - study
Just under 6% of England’s population – around 3.4 million people – had been infected with coronavirus by the end of June according to an estimate based on antibody tests.
More than 100,000 people tested themselves for antibodies against the SARS-CoV-2 virus that can lead to COVID-19.
The results from the study by Imperial College, London, have yet to be peer reviewed but are available in a report published online.
London had the highest numbers at over twice the national average (13%), while the South West had the lowest (3%).
Key workers in care homes and health care were among those most likely to have already been infected with the coronavirus.
Black, Asian and minority ethnic (BAME) individuals were between two and three times as likely to have had COVID-19 compared to white people, the study showed.
The overall infection fatality ratio – the proportion of infected people who died – was calculated to be 0.9%, similar to other countries such as Spain.
Antibodies were found in almost all (96%) of those who had a previous infection confirmed by a swab test.
People who had severe symptoms from the disease were twice as likely to have antibodies than those with no symptoms when they were diagnosed with or suspected having COVID-19 (29% vs 14%).
The highest numbers of positive results were in people who reported confirmed or suspected COVID-19 in March and April, and were shown across all regions of England.
More than 16% of care home workers with client-facing roles and 12% of healthcare professionals that have direct patient contact had positive results. In non-key workers, the rate was around 5%.
For Black, Asian and other ethnicity individuals, the rates of positive results were 17%, 12% and 12%, respectively, compared to 5% for white individuals.
The gap was reduced after the researchers took into account factors such as age and key worker status, but rates were still higher overall for BAME individuals.
Other factors not explored included transport use and behaviour, authors said.
Young people aged 18-24 had the highest rates (8%) and were more than twice as likely to test positive than adults aged 65 to 74, who were least likely to have the virus (3%).
Authors said that understanding trends and geographical variations could help guide local public health responses, identify groups at risk and inform actions to control the disease.
The REACT study was commissioned by the Department of Health and Social Care and is being carried out in partnership with Imperial College London, Imperial College Healthcare NHS Trust and Ipsos MORI.
The study will be repeated in the autumn, testing 200,000 people, and research on the accuracy of different tests is ongoing to ensure that the best available test is used as the programme continues.
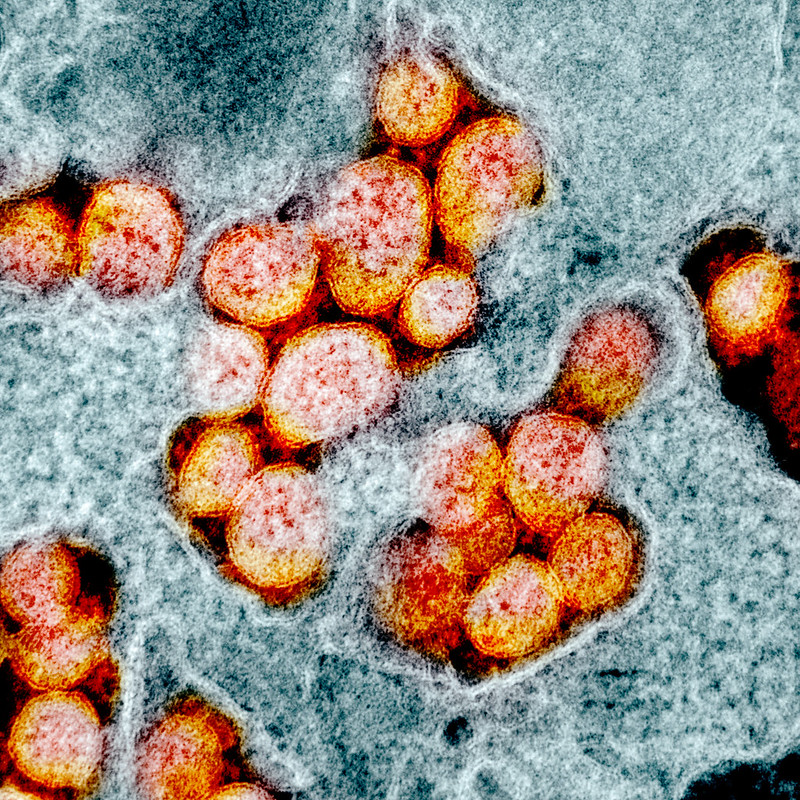
Feature image courtesy of Rocky Mountain Laboratories/NIH











