NHS under fire for rationing hep C drugs
England’s National Health Service is limiting access to expensive hepatitis C drugs – despite NICE ruling that they are cost-effective and should be funded, according to an investigation.
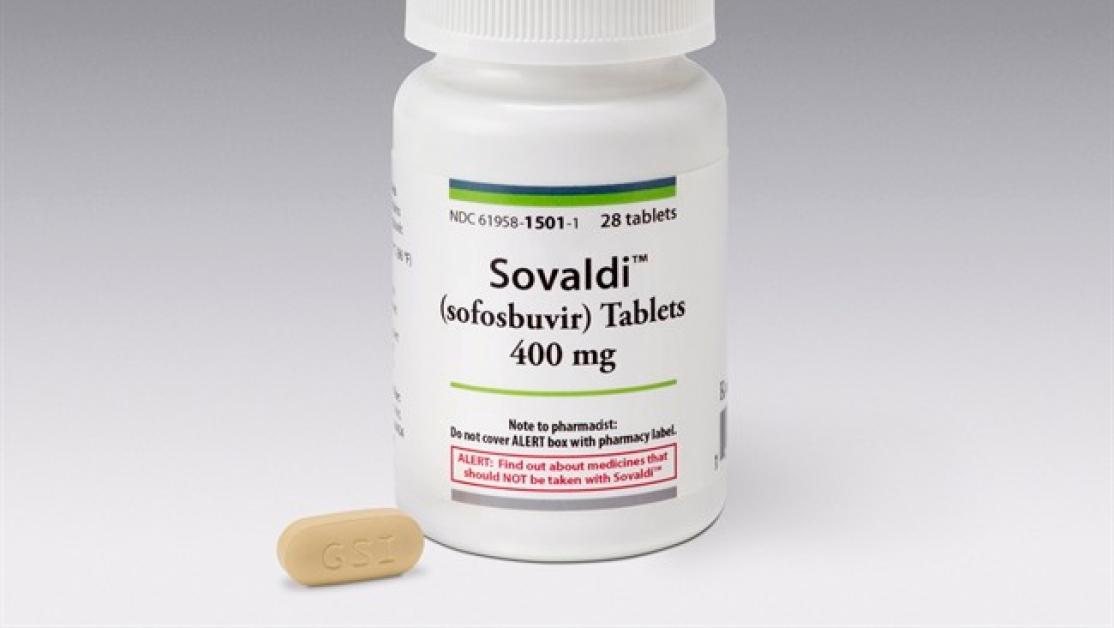
The row centres around Gilead’s Sovaldi (sofosbuvir), priced at almost £35,000 per course in the UK.
Despite its high cost, NICE has ruled that Sovaldi and other hepatitis C drugs are worth paying for because, as they cure the disease, they bring long-term savings to the NHS.
NHS England is facing intense budget constraints - and a joint investigation by the British Medical Journal and the University of Cambridge and the University of Bath found the organisation fought to avoid paying for Sovaldi.
When NHS England failed to influence NICE’s assessment, it “defied NICE’s authority” by rationing access to the drugs.
NHS England was also unable to bargain for a lower price from Gilead because of legal arrangements for procurement, the investigation found.
Last year, NICE recommended Sovaldi and later Harvoni (sofosbuvir+ledipasvir), as well as competitor treatments from AbbVie and Bristol-Myers Squibb.
NHS England successfully delayed funding for 90 days beyond the standard three-month grace period following NICE final guidance.
It then attempted to block Harvoni and competitor drugs by questioning the level of evidence, although NICE eventually prevailed and published guidance recommending funding late last year.
Despite the NICE guidance, NHS England has restricted use of hepatitis C drugs by imposing quotas on clinical teams across the country, the BMJ said.
The article quoted Steve Ryder, a hepatologist from Queen’s Medical Centre, University of Nottingham, who said patients turning up at clinics early in the month are more likely to get immediate treatment, because of the spending constraints.
The BMJ also investigated why NHS England has been unable to obtain a discount from Gilead. A company spokesperson said procurement arrangements mean only the Commercial Medicines Unit, accountable to the Department of Health, is able to negotiate regional discounts with pharma companies.
Claims dismissed as 'inaccurate and naïve'
But NHS England said the claims in the article are “inaccurate and naïve”.
In a statement a spokesperson said the NHS had invested £200 million in hepatitis C treatments last year, and again this year, the single biggest new treatment investment in years.
High-risk patients were treated first, and the NHS is “now working through the backlog of non-urgent patients.”
The spokesperson added: “It is utterly naïve to pretend that the NHS could instead somehow have 'magicked up' several billion pounds in one year, for this one condition, without that meaning damaging cuts in other critical services such as mental health, cancer or primary care. That’s not a failure of planning; that’s just the reality of the financial circumstances facing us.”











