How to improve patient outcomes with digital health

Digital health solutions that work in the real world must also be designed to effectively support the patient’s tasks and goals, while being engaging to use. In other words, they need to be built with patients, not for them, say Alex Butler and Gavin Birchnall.


Alex Butler (left) and Gavin Birchnall
There is currently a great deal of focus on patient centricity within the pharmaceutical industry. Most industry stakeholders now believe that one of the most exciting opportunities for healthcare is the development of digital health technology that can manage disease, improve outcomes for patients and positively support healthcare professionals to improve the provision of care.
It is commonly agreed that in order to be effective, these solutions need to be truly built around patients and their needs. The concept of patient-centred design is now becoming part of mainstream discussion. However, this goes much deeper than simply designing a user-friendly interface. Solutions that work in the real world must also be designed to effectively support the patient’s tasks and goals, while being engaging to use. In other words, they need to be built with patients, not for them.
This starts with truly understanding patients’ problems through in-depth research and analysis. It is important that any pharma-sponsored support programme aligns with strategic objectives but also rigorously meets real patient need and is differentiated from currently-available solutions. Building the value proposition should be done collaboratively, and through a process of co-creation. When patients truly partner with clinicians, academia, pharma and health technology experts, the results can be incredible.
Building a value proposition
When identifying a digital health solution to support patients with a chronic disease, a value proposition model should be used as a foundation tool for collaborative patient support design (figure 1):
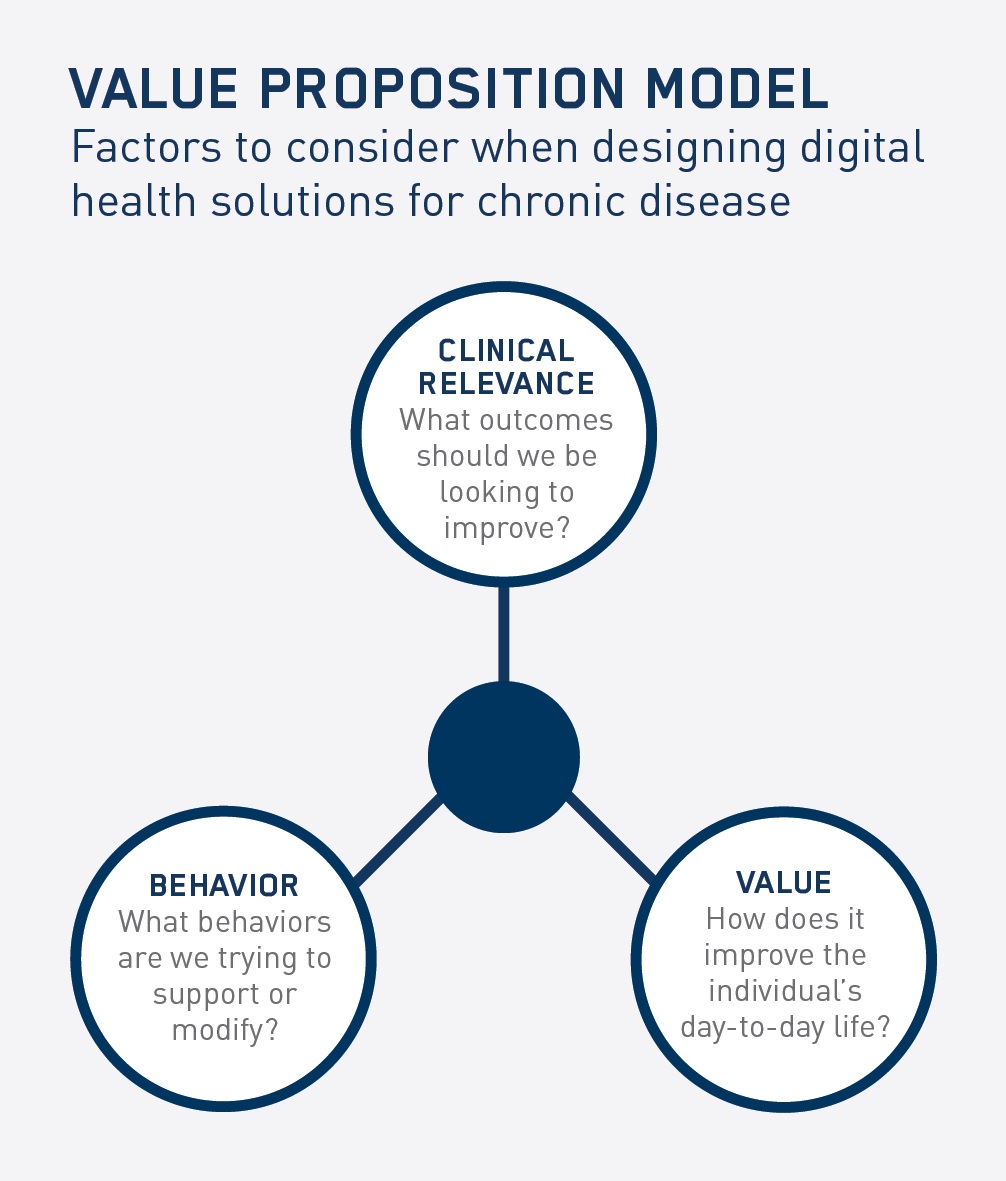
Figure 1: Value Proposition Model: Factors to consider when designing digital health solutions for chronic disease
Clinical relevance
It is essential that digital support tools address validated needs and produce evidence to measure improvements in clinical outcomes for real people living with any acute or chronic condition. To do this, we must align with significant clinical interventions that work beyond the medicine’s clinical effectiveness. The objective of a support programme should be greater than simply focusing on adherence or providing disease information. Solutions need to solve real problems and lead to improved patient experience and quality of life.
Behaviour
The focus for any digital health solution should be on the desired behaviours being sought, not the technology itself. This requires building any interventions on a sound foundation of behavioural science. Human beings are not primarily rational in how they make decisions; this is no different when it comes to health. However, most information and services in healthcare are built on the basis that people make only rational decisions. Therefore programmes should be created with motivational design at their core.
User value
It is imperative that a solution provides genuine value to the user; this needs to be the primary objective of any digital health strategy. The solution should integrate with a person’s everyday life and provide support within the context of everyday activities too. Anything that makes managing a condition more time consuming or confusing simply won’t be used ─ as many available websites, tools and applications demonstrate. Although it seems obvious, this focused attention on the user value is not always easy for pharma, healthcare professionals (HCPs), or academics. Finding the sweet spot of mutual value is the key to success.
Empowering change
We recently ran a workshop to look at how this value proposition model can be applied to some of the key challenges facing healthcare in the 21st century. Chronic diseases, such as COPD, diabetes, stroke and cancer, are by far the leading cause of mortality around the world. They also have an extremely detrimental effect on people’s quality of life. During the workshop, groups comprising patients, HCPs and pharma professionals applied the value proposition model described above to begin the process of collaborative patient support design. The groups put forward interesting solutions, two of which are detailed below:
Empower diabetes patients to use technology to learn how their body responds to food, drink and exercise
Patients with type 2 diabetes often struggle with managing their HbA1c levels and regularly monitoring blood glucose levels in order to maintain health and avoid complications/co-morbidities. Advances in blood glucose monitoring, such as the FreeStyle Libre from Abbott, eliminate the need for patients to perform finger-prick tests to monitor their blood glucose levels, instead scanning a sensor on their arm.
The group saw that, in addition to being highly convenient, the device has the potential to produce data that can help the individual learn more about how their body responds to food, drink and exercise. Their solution was to make this device more than just a data collection tool, but to use it as a learning tool that provides instant feedback to the user, suggests improvements, and provides helpful tips and advice (even encouragement from a coach). While the information would be available for the HCP to view, the group felt that it was about empowering the individual and using technology in a highly personalised way to help the person lead a healthy life.
Help patients when they need it most: An example in cancer
The shock a patient experiences upon being diagnosed with cancer is well documented. Many patients report that they heard very little of what their HCP said after they heard the ‘C word’. Faced with this diagnosis, many patients struggle to understand the disease, their treatment options, and available means of support.
The group debated the need for better information and advice in the first seven days after diagnosis. One patient spoke of her doctor, who advised that she should not look online. Whether or not the intent was to protect her from potentially frightening information, it meant that the treatment path was designed for the patient, not with the patient.
In this scenario, a digital health solution could serve the purpose of providing patients with access to high quality information, personalised to their condition and their learning preference. This would go a long way towards enabling patients to understand their options and actively participate in treatment decision-making alongside their HCP, rather than being told which path to follow.
Reflections
The examples presented here stress the need to create digital health solutions with patients, not for patients. The cancer example illustrates that only when you understand and walk the path of the patient can you truly impact lives. It also demonstrates that when thinking about how to support patients, it should never be with an agenda (such as how to improve adherence or collect more data).
The diabetes solution was also interesting as it builds on an existing platform and technology (progress isn’t about reinventing the wheel). The blood glucose result is built on clinically-relevant measures, but takes these further to drive behaviour by using the result(s) to provide instant user feedback. The result suddenly goes from a ‘number’ to a sequence of positive interventions with the individual’s needs front and centre. The value to the user could be immense as a companion to maintaining health, rather than simply providing a static result.
True patient support is about understanding, recognising and solving real problems and aiming to improve individual health. This is the ultimate goal of everything we do. Hearing it first-hand is always insightful and powerful.
About the authors:
Alex Butler is co-founder of Foundry3 and Gavin Birchnall is director, Digital Patient, at ERT.
Alex Butler has led the digital transformation of healthcare for the past 15 years, both from within the industry at Johnson & Johnson and servicing the industry by founding and leading multiple award-winning agencies. Most recently he co-founded Foundry3, which incorporates a digital health innovation lab focused on the pharmaceutical industry: the Innovation Foundry.
Gavin Birchnall applies his passion for driving the advancement of digital health through the design and development of integrated health platforms that improve patients’ lives. He has a strong background in the clinical and healthcare technology industry, including nearly 20 years’ experience in project and product management for some of the world’s largest global solutions providers. He has presented and published numerous articles on best practices for improving health outcomes through the use of effective digital health and patient support programmes.