Depression, alcohol and drug problems: the hidden toll of HIV

David Rowlands examines the results of his most recent poll on standards of psychological care in HIV – an important factor as 96 per cent of respondents agreed that those living with HIV experience significantly higher rates of depression than the general population.
According to the British HIV Association (BHIVA) Standards of Care for People Living with HIV, those affected by HIV have far greater rates of depression and other psychological problems than the general population. This has a major impact on quality of life, complicates clinical care, compromises physical health and heightens the risks of onward HIV transmission. Therefore, promoting good mental health and wellbeing for people with HIV is of critical importance.
The standards report states that 'appropriate and timely psychological support is an essential component of good clinical care. People with HIV should have access to services that assess emotional and psychological well-being, detect potential psychological problems and plan appropriate interventions in terms of stepped-care interventions that are delivered by appropriately qualified providers.'
The BHIVA worked in partnership with care providers, professional associations, commissioners and people living with HIV, to produce the quality standards, which cover 12 key themes, encompassing the most important issues for the care of people with HIV. Derived from the best available evidence, they focus on aspects of care that have particular relevance for delivering equitable high-quality services that secure the best possible outcomes for people with HIV.
Standard 6 focuses on psychological care and states: 'People living with HIV should receive care and support which promotes their mental, emotional and cognitive well-being and is sensitive to the unique aspects of living with HIV.'
One of its quality statements reads: "People living with HIV should be screened for the presence of symptoms of depression, anxiety, drug and alcohol misuse, acute stress disorder, risk of self-harm and cognitive difficulties within the first three months of receiving an HIV diagnosis."
"Standard 6 recognises that screening is valuable for identification of psychological problems and cognitive impairment"
Standard 6 recognises that screening is valuable for identification of psychological problems and cognitive impairment, adding that 'it should be repeated annually and following events known to trigger or exacerbate psychological distress or cognitive difficulties, such as significant changes in physical health or disease progression, starting antiretroviral therapy, difficulties with adherence and returning to clinical care after being lost to follow-up.' It lists other triggers, including significant life events such as a difficult relationship break-up, experiencing stigma or violence, losing benefits or a sudden death of a loved one.
'Screening can range from brief questions ... and move to more complex tools, such as validated questionnaires and cognitive tests, depending on the response to initial screening questions. For someone who is not experiencing any difficulties, screening might be limited to one or two questions. For those where there are concerns, screening can be escalated, with appropriate onward referral and appropriate support services for their needs.'
Responding to the poll, Ken, 27, from Manchester said: "When I was first diagnosed two years ago with HIV, I found it hard to communicate with my HIV support team about my drug and alcohol misuse. I therefore aimed to establish a strong network of like-minded people like myself, using social media and online forums to discuss my mental and physical health. Over time this has improved my knowledge, confidence and has enabled me to better engage within my care"
Standard 6 continues: 'The stepped-care approach (Figure 1) could be used to enable access to the appropriate psychological support services and cognitive rehabilitation needed by each individual. This provides a framework for comprehensive assessment and provision of psychological support to meet the range of needs of people living with HIV. While the particular services available locally may determine how such support is provided and by whom, all aspects of assessment and support described in the model should be available regardless of geographic location in the UK.
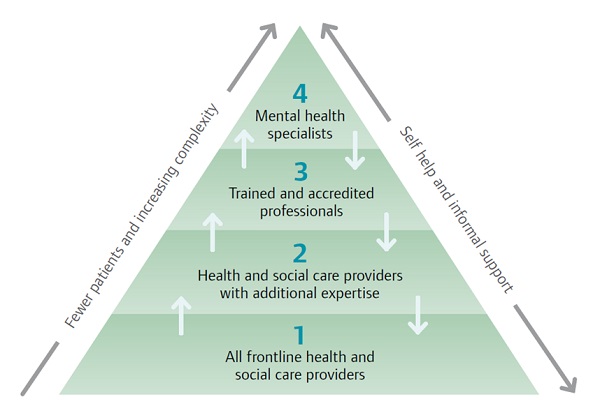
Figure 1: Stepped-care approach model
'Clear pathways should be defined between those services providing HIV clinical treatment and those offering psychological support. Psychological support may need to be delivered through a network of providers with a variety of expertise and should include access to local mental health services, including psychiatric and community support, and be linked to social services and services for managing the functional impact of psychological difficulties. Services should be planned to provide seamless integration across the various levels of psychological support, including transitions between services for people of all ages living with HIV.'
Our recent poll on this subject showed that 96 per cent of respondents agreed that people living with HIV experience significantly higher rates of depression and other psychological problems.
"I believe psychological support services should be high-quality, accessible, needs-based and strategically planned"
I believe psychological support services should be high quality, accessible, needs-based and strategically planned with clearly defined and accountable leadership and management arrangements. Clinical leadership should be provided by practitioners who have psychological support skills with particular expertise in HIV. Clinical leads should be part of the multidisciplinary team providing HIV care, communicate effectively and collaborate with the professional leads of other services providing psychological support for people living with HIV e.g. social care, voluntary sector and working closely with commissioners.
'Practitioners need to demonstrate their competence on an ongoing basis,' the Standards state. 'Services should support the maintenance of such competencies through training, continuous professional development and supervision. All practitioners should be able to display a minimum set of competencies demonstrating their awareness and understanding of HIV and its impact on those living with the disease. They should possess an awareness of the diversity of needs that people living with HIV may have.'
Sandra, 53, from London, diagnosed 14 years ago, said: "I believe that we all have a responsibility to make people aware and better understand about living well and long with HIV. I often speak at GP practices, support groups and HealthWatch meetings. This improves people's knowledge, understanding and breaks down stigma. I feel sharing my experiences not only benefits others, but also myself."
Poll data
The poll received a total of 116 respondents between 15 April and 4 May 2015, with data collected via online hosting at www.Design-Redefined.co.uk and social networking sites. Thanks go to the community for their input.
The next poll examines if people living with hepatitis C should access treatment now, or wait for emerging therapies. View the poll and vote here.
About the author:
David Rowlands is the director of Design-Redefined.co.uk, delivering effective healthcare communications to professionals and patients.
His key objective is to design, develop and deliver community projects to enable people living with, or affected by, HIV and/or Hepatitis C (HCV) to become better engaged with their treatment and care.
Working over a number of media platforms, across the public, private and third sector, he is able to establish a link to these sometimes hard-to-reach communities.
Contact David on Email: david@design-redefined.co.uk , Website: www.design-redefined.co.uk, Twitter: DR_tweetUK
Read the results and analysis of the previous poll:











